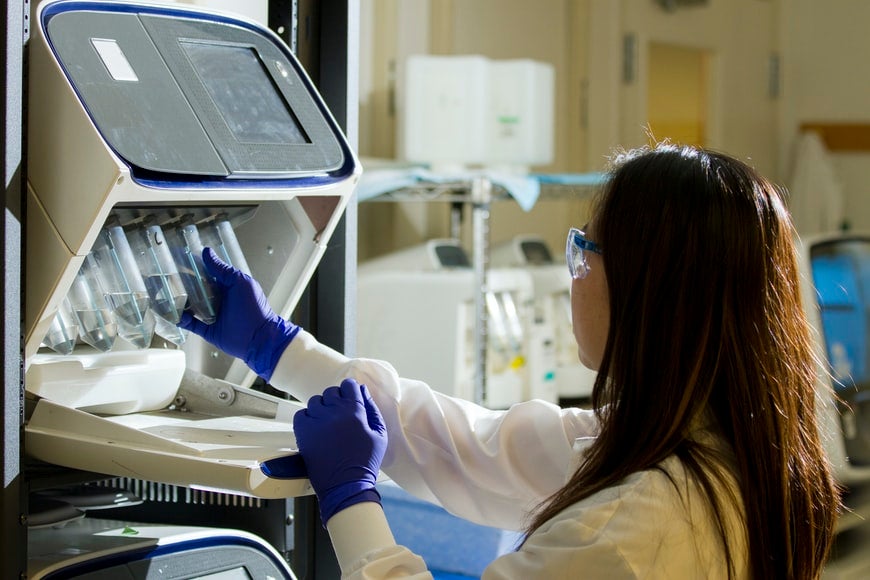
Medical devices look a lot different today than they did just two or three decades ago, and the process of designing and manufacturing them has changed in kind. Owning or operating a medical device company requires a new understanding of a variety of concepts, from biocompatibility to the industrial internet of things and how smart technology and 5G networking can change the way the medical industry looks at implantable devices.
As technology has changed, the medical industry’s capabilities have advanced exponentially. As new devices emerge, the need for biocompatibility, or a material’s compatibility with living tissue, has also increased. What does it take to determine the biocompatibility of medical device components?
Combining Engineering and Toxicology
The ideal addition for your team, if biocompatibility is a concern, is a biocompatibility toxicologist. These professionals combine the best of both worlds and usually have degrees in both engineering and toxicology. This enables them to understand not only how potentially toxic materials could affect the body, but how to engineer the devices to use non-toxic or biocompatible materials.
Having a biocompatibility toxicologist on your team prevents biocompatibility issues from hiding until late in the production and design process. Biocompatibility studies often don’t happen until the submission writing stages, and by then it’s far too late to go back and fix the problems without tearing down the whole design and recreating it from the ground up.
Exploring Various Biocompatibility Testing Methods
The concept of biocompatibility testing isn’t a new one, though the FDA’s compatibility guidelines weren’t published until 2016, and any companies that ship their devices internationally also have to adhere to the ISO 10993-1-2018 standards as well. Let’s take a look at some of the more common biocompatibility testing methods.
External Tests (Cytotoxicity, Sensitization Assays, Irritation Tests)
Not all medical devices are designed for internal use, but they still need to be biocompatible to prevent sensitivity issues, irritation on the skin, and allergic reactions. That is where these external tests come in.
Cytotoxicity tests rely on tissue cultures to assess toxicity, using materials of various densities as well as different extracting media to determine biocompatibility. Sensitization tests focus on whether a material will build up in the tissues, causing sensitivity over time, and irritation tests focus on whether the material may cause irritation of the skin or mucus membranes.
Toxicity Assessments (Acute Systemic, Subchronic, Genotoxicity, Reproductive & Developmental)
A material might pass the initial testing types that we listed above, but that is just the first stage. The next steps explore what it would take to make a substance toxic.
Acute system toxicity tests extract leachable chemicals — those that can leech out of material — and inject them into test animals to see at what concentrations they become toxic. Subchronic toxicity tests focus on longer-term exposure, exposing the test subjects for up to 10% of their total expected lifespan.
Genotoxicity testing looks for mutagens that could potentially cause cell damage. Prolonged exposure to these mutagens increases the risk of cancer as well as inheritable genetic defects.
Finally, as its name suggests, reproductive and developmental testing focuses on how a substance could potentially impact reproduction as well as the birth of new children.
Hemocompatibility
Hemocompatibility is necessary for any device that will come into contact with a patient’s blood, both for short-term procedures and long-term implantation. This means it needs to remain neutral when exposed to blood, and cannot affect coagulation or other functions of the body’s cardiovascular system.
Carcinogenesis Bioassay
We’ve mentioned the potential for the creation of mutagens, but that isn’t the only thing in medical device creation that could cause cancer. Each material needs to be assessed to determine whether or not it creates or emits carcinogens before or after it is installed in the body.
Implantation Tests and Histopathology
Once the material has passed the previously mentioned tests with flying colors, it is time to move on to implantation tests and histopathology. As the name suggests, implantation tests involve implanting the material or device into living tissue for an extended period of time. After that period passes, the testing moves on to histopathology.
Both the implant and tissue are removed and assessed under a microscope to ensure there are no problems that could impact the device’s biocompatibility. Histopathology is used in a variety of different forms of diagnostic medicine and has become a valuable tool for determining a substance’s biocompatibility.
Pharmacokinetics
Pharmacokinetics, also known as Absorption/Distribution/Metabolism/Excretion, or ADME, is a broad umbrella used to look into the metabolic absorption of various materials in the medical industry. This testing is primarily used for bioabsorbable materials such as dissolving stitches or treatments that pair drugs and devices.
Preclinical Safety Testing
This is often the final stage of testing before a device is eligible for human trials and studies. The exact details of preclinical safety testing will vary depending on a number of factors, including the device itself, all the included materials, and the task it is designed to complete.
Why Is Biocompatibility Important?
Biocompatibility is an essential part of the medical industry. These devices are designed to remain in the human body for months or even years. Some, such as implantable pacemakers and defibrillators, only need to be replaced when their batteries die. Others, like joint replacements, are designed to be permanent and will remain within the patient’s body until the day they die.
Medical professionals cannot implant these devices with any confidence unless they can ensure the materials they’re designed from are 100% biocompatible and won’t cause more problems than they solve. The science of biocompatibility isn’t perfect, but it is constantly evolving and improving. Even without perfection, the goal is to create medical devices that are safe to implant in the human body, and in most of our attempts, it’s safe to say we succeeded.
2828 Views